blog
October 3, 2024
Menopause Weight Gain: Why It Happens and What to Do
“It felt like the weight gain appeared overnight, all around my middle, and nothing seemed to shift it even when I tried eating less and spending even longer at the gym”
Sound familiar? You’re not alone.
Menopause related weight gain is such a common struggle, leaving many women frustrated and confused. Suddenly your body isn’t behaving the way it used to, and that can be daunting.
When I first meet clients, they often blame themselves for their weight gain. They think they lack the willpower or they don’t have what it takes to make a difference.
When we feel frustrated or uncertain, we tend to blame ourselves, compare to others, or chase quick-fix diets that rarely work long term.
However, the truth is, it’s not your fault. And it’s not about trying harder or having more willpower.
There are additional reasons during menopause that can explain what’s happening. It is normal for our body to change during midlife but understanding why can be helpful as it can move us away from self-blame and empower us to focus on a mindset and actions that can make a difference.
How Common Is Menopause Weight Gain?
Around 70% of women experience weight gain during the menopause transition and cite this as one of their main concerns.
Research shows the rate of fat gain doubles during perimenopause, often coinciding with muscle loss. On average, women gain about 1 lb per year during this time which can add up over the duration of the menopause transition. For many women, this rate of fat gain slows down post-menopause, although this isn’t always the case.
Menopause Weight Gain Causes: Why Does It Happen?
There isn’t a single reason for weight gain during menopause, or at any other time in our lifespan, and each woman’s experience is unique.
Factors such as health background, medical conditions, lifestyle, stress levels, medications and genetics all play a role. Plus, we are living in a world where the healthier choices are the more challenging.
Midlife can also be a time of specific emotional and/or practical challenges; caring for elderly relatives, children leaving home or relationship difficulties, which occur alongside hormonal changes and can make managing weight difficult leaving us with little time or energy for self-care.
No one’s situation is the same. For some women, weight becomes a new challenge during perimenopause, while for others, long-standing struggles can intensify at this stage.
Despite all these different factors there are some reasons specific to menopause that its helpful to consider. Let’s explore these in more detail.
Hormone Shifts and Oestrogen Changes That Drive Menopause Weight Gain
As we know oestrogen levels fluctuate during perimenopause and it is this chaoti pattern that triggers many of our symptoms.
One of oestrogens jobs in the body is to tell it where to store fat. In our younger years it’s directed to our thighs and hips, which is a healthy storage place. But as our hormones change and oestrogen drops more fat is stored around the stomach.
This shift in where fat is stored can be very frustrating when our clothes don’t fit as they used to but also because deep abdominal fat (visceral fat) is linked to poor insulin sensitivity (see below) and higher risks of conditions like type 2 diabetes, fatty liver disease, and heart disease.
Insulin Sensitivity and Midlife Metabolism
For some women lower oestrogen levels can also make the body less sensitive to insulin’s action and may lead to insulin resistance.
One of insulin’s jobs in the body is to move sugar out of the blood and into the cells where it’s needed to make energy. When we’re insulin resistant the cells stops listening to this message so we make more and more insulin so the message is louder and sugar is forced out of the blood and into the muscles.
These high insulin levels can lead to more fat storage and weight gain and a viscous cycle can develop. Insulin resistance drives weight gain and weight gain leads to more insulin resistance unless we focus specifically on how to increase insulin sensitivity in the body.
Too much fat around the middle releases substances that trigger chronic inflammation, which in turn increases insulin resistance.
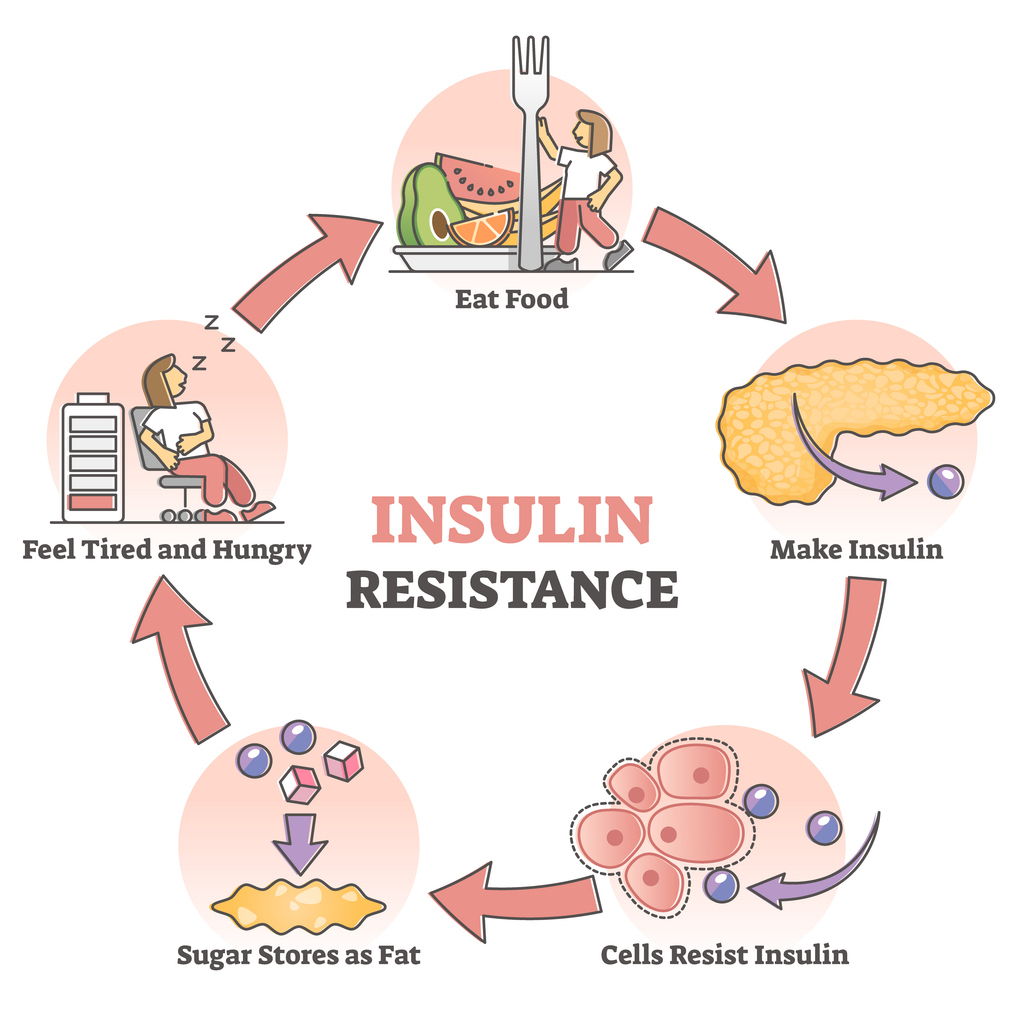
Eventually (usually after years) the body can’t keep up with the need to make more and more insulin and so blood sugar levels rise and this is the start of type 2 diabetes.
Understanding the link between storing fat around the middle and insulin resistance is important because it helps us focus on the lifestyle choices that help to increase the bodies sensitivity to insulin.
Fat stored in the liver and pancreas
Fat that sits just beneath the skin is known as subcutaneous fat. It’s the stuff we can pinch between our fingers and it’s the healthy place to store it.
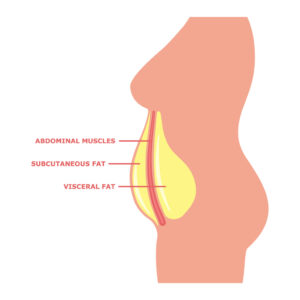
In recent years we’ve come to understand that everyone has their own ‘personal fat threshold’ which is the level of fat in the body that can be healthily stored under the skin. If we go above this threshold, fat begins to be stored in and around organs like the liver and pancreas and interferes with how they work. Too much fat in the liver and pancreas increases the likelihood of insulin resistance and eventually of developing fatty liver and type 2 diabetes.
Why Hormonal Changes Trigger Cravings
Oestrogen helps regulate appetite, and as oestrogen drops, many women experience increased hunger and cravings. Disrupted sleep, a common menopause symptom, can exacerbate this by increasing hunger hormones and cravings, particularly for sugary or high-carbohydrate foods.
Muscle Loss and Metabolism in Midlife
As we age, we naturally lose muscle at a rate of 1-2% per year. We may notice these changes as we move through perimenopause. Maybe we’re not as strong as we used to be, we don’t have the same muscle definition, or we can’t do activities in the way we used to.
Protecting and preserving our muscles is extremely important when we’re thinking about managing weight and health but also because of how it shapes our future risk of frailty and quality of life in later years.
Muscle is metabolically active tissue, meaning it burns more energy (calories) than fat, even at rest. So the higher our muscle mass the higher the body’s metabolic rate and the more energy (calories) the body will burn at rest which clearly is helpful for our body composition and weight.
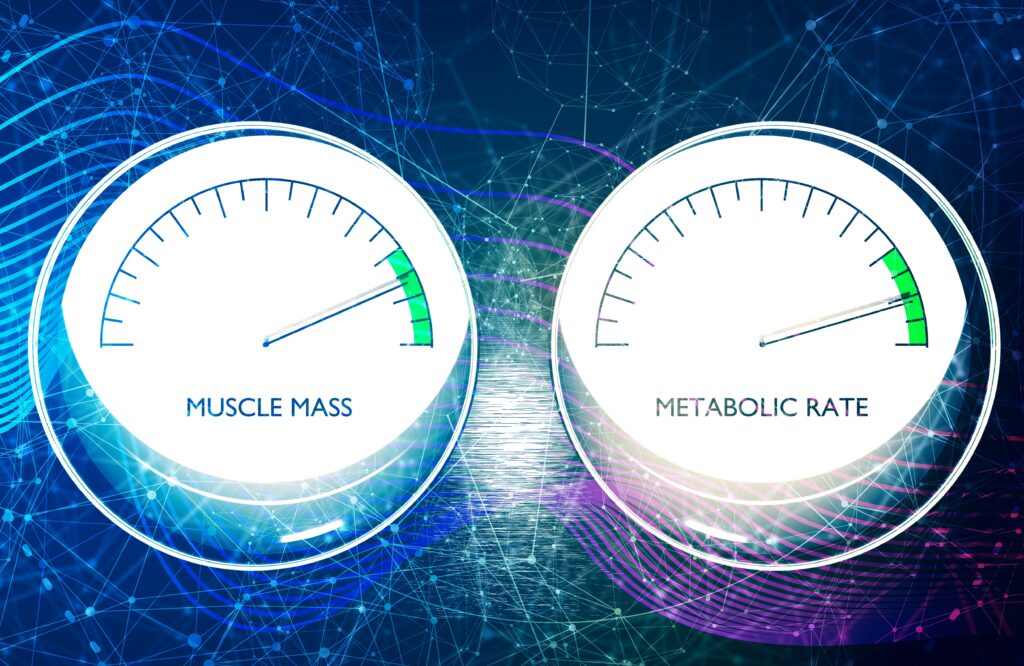
Improved muscle health also improves insulin sensitivity so we can limit the risk of insulin resistance and all the downstream effects this can have (type 2 diabetes, fatty liver and cardiovascular disease).
So when we’re thinking about managing weight, where muscle loss can be an unintended consequence, we need to consider strategies that will optimise muscle health and preserve and build muscle. This is why combining dietary changes like optimising protein intake, ensuring adequate fibre together with resistance training and aerobic activity is so important.
The Sleep Weight Connection.
Insufficient sleep (generally 7 hours or less) and/or poor quality sleep, often experienced during the menopause transition, are linked with weight gain and poor metabolic health.
Sleep deprivation increases hunger hormones, decreases insulin sensitivity and reduces activity the next day. Poor sleep often leads to less healthy food choices and stronger cravings for sugary and salty snacks.
We all know that feeling after tossing and turning all night when only a sugary snack and a strong coffee seems to hit the mark.
And the science shows its not all in our heads. We’re less likely to opt for fruits, vegetables and high fibre foods and more likely to turn to sugary and salty foods in part due to changes in hormones that control appetite.

Recognising the link between poor sleep and how it affects our eating and activity habits is important but improving sleep quality and quantity can be particularly difficult for some women during the menopause transition.
Focusing on our sleep hygiene can be a helpful first step (check our this website for help with all aspects of sleep) but if sleep continues to be elusive and its impacting your health and progress its worth having a conversation with your doctor.
It’s also helpful to think through how we’re responding to tiredness and low energy and whether some of our coping strategies might be making sleep less likely going forward. The amount and timing of caffeine and alcohol can be a useful starting point to consider.
How Stress Affects Weight
Midlife often brings new stressors—whether it’s managing a challenging career, caring for aging parents, children leaving home or other life difficulties.
Stress has been linked to weight gain with increases in hunger hormones and changes to what we eat with higher amounts of ‘comfort’ foods. The effects of stress on eating and weight seem to differ depending on the type of stress and how long it lasts.

We may lose our appetite during bouts of acute stress but long term stress encourages us to want and seek out highly palatable foods which may be due to higher levels of the stress hormone Cortisol. This hormone has also been linked with increased insulin resistance and fat storage although this is complex and not fully understood. Relaxation techniques can help manage chronic stress, improve weight loss, and lift mood and anxiety.
How to Stop Menopause Weight Gain: Steps That Make a Difference
We’ve explored the importance of protecting our muscles and their health, the role of insulin resistance, the value of maximising sleep quality and quantity as well as managing the stress in our lives.
So how can you start making changes that truly help?
To protect muscle health
- Focus on Protein-Rich Meal
Protein helps preserve muscle during weight loss, which supports a healthy metabolism. It also reduces hunger and keeps you fuller for longer. Include lean proteins like chicken, fish, tofu, tempeh, pulses/beans, and eggs in every meal to support muscle maintenance and satiety.

- Incorporate Activity & Strength Training
Strength training is one of the most effective ways to combat muscle loss during menopause. Include resistance exercises like weights, bodyweight moves, or bands to maintain muscle, boost metabolism, and prevent weight gain.
Even short activity helps. A 10–15 minute walk after meals can quickly improve insulin sensitivity.

To improve insulin sensitivity
- Eat Plenty of High Fibre Foods
Fibre-rich foods like vegetables, fruits, grains, and beans support gut health. They balance blood sugar and keep you fuller longer.
- Limit Refined Carbs and Sugar
Eating less refined starchy and sugary foods helps manage insulin sensitivity and prevent fat storage around the middle. Opt for whole grain starchy foods where possible.
- Prioritize Sleep and Stress Management
Quality sleep and stress management are just as vital as nutrition and exercise. Prioritise good sleep, mindfulness, and activities that bring you joy and calm.
Menopause Weight Gain: The Bottom Line
Although changes in weight and shape are common in menopause there are many things we can do to make a difference to how we feel now and in the future. While some of these can be challenging the right support can make all the difference.
Making changes in midlife doesn’t have to feel overwhelming. If you’d like some personalised support to get clear on what will truly help your habits, health, and weight, take a look at my Work With Me page to see how we can work together.